No private company should have monopoly rights over a Covid-19 vaccine; this is a public resource that should be contributed to the World Health Organisation’s Technology Access Pool and shared for the benefit of all, writes Helen Clark and Winnie Byanyima.
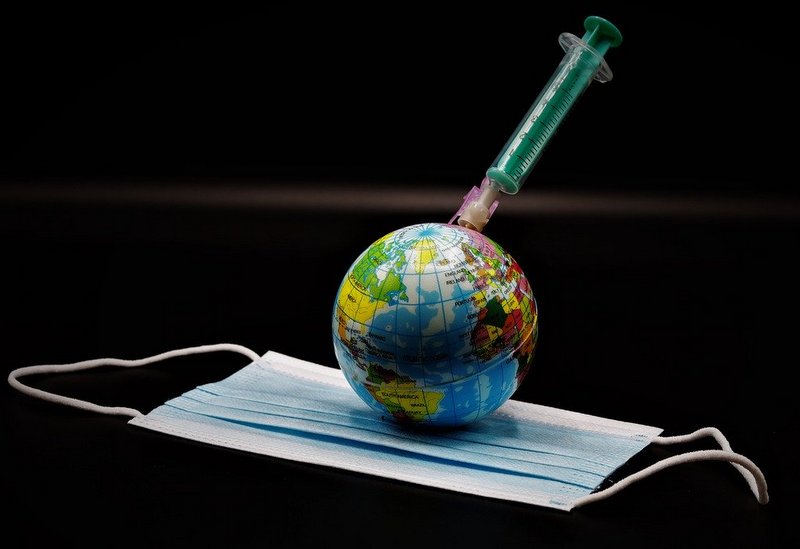
To bring an end to the pandemic, the world needs a vaccine. Promising early trial results for the vaccine developed by Oxford University suggest we’re inching closer to discovering one.
Data published recently in the Lancet shows the Oxford vaccine produced antibodies and T-cells in roughly 1,000 patients. The pharmaceutical company, AstraZeneca, has been licensed to produce this vaccine by early 2021, which includes an agreement to produce 1 billion doses with the Serum Institute in India for low- and middle-income countries by the end of that year.
But this is still a long way from what is needed. To vaccinate everyone, the world needs as many as 7.8bn doses, as quickly as possible. If the successful vaccine requires more than one dose, or must be given annually, as seems likely, the figure will be higher still. The world will need a near-permanent supply of the vaccine. Only then can we bring Covid-19 under control.
Once a safe and effective vaccine is discovered, the only barrier to providing sufficient doses should be the world’s manufacturing capacity. But other artificial barriers stand in the way. The intellectual property laws that grant pharmaceutical companies the exclusive rights to produce a particular medicine for a certain number of years are intended to reward investment and innovation into new medicines. These intellectual property rights are often abused and create monopolies, and in the case of the Covid-19 vaccine they threaten to limit the supply, causing deadly shortages and unnecessary delays.
Granting one company exclusive rights to the science, knowhow and intellectual property of a coronavirus vaccine will prevent us from getting the billions of doses that the world needs. No private company, however committed it might be to delivering a vaccine, should have a monopoly over this public resource. A global pandemic is not the time to artificially ration the supply of a medicine because of failed ideas about the sanctity of intellectual property. Nor should the market be protected simply to serve the interests of pharmaceutical corporations.
It’s also important to remember that AstraZeneca didn’t discover this vaccine. Billions of dollars of taxpayers’ money have been poured into the development and production of a Covid-19 vaccine. AstraZeneca has received $1.2bn from the United States government alone, and at least £84mfrom the UK government. Nor is the company bearing the risks of this innovation alone: governments are already committing to purchase the vaccine in advance of its production.
In the rush to solve the global challenge of finding a Covid-19 vaccine, the leaders of rich countries appear to be relying on the goodwill of companies and a charitable approach towards poor nations and ignoring the barriers that intellectual property and other monopolies present. They seem to be assuming that the only option available is a private, market-based approach directed and controlled by pharmaceutical corporations. As the president of South Africa, Cyril Ramaphosa, and prime minister of Pakistan, Imran Khan, made clear recently when they joined 140 other public figures in calling for a “people’s vaccine”, this would be a grave mistake.
Current distribution plans for the Oxford vaccine are an alarming reminder of what happens when you leave a public resource in the hands of a single company. Around 300m doses have been promised for developing countries by the end of this year – a welcome step, but one that pales in comparison with the 400m doses that will go to the US and UK. The Netherlands, Italy, France and Germany have secured another 400m doses between them. The EU and other rich nations are also pushing their way to the front of the queue. Many middle-income countries, such as those in Latin America, where the scale of the outbreak is frightening, may be completely locked out of these arrangements.
When the American virologist Jonas Salk was asked who owned the patent to the polio vaccine he invented, he famously replied: “There is no patent. Could you patent the sun?” Oxford University should heed his remark and show leadership by contributing its knowledge and intellectual property to the World Health Organization’s Covid-19 Technology Access Pool, where technology and treatments are shared for the benefit of all. Likewise, governments and charitable foundations that are funding promising vaccine candidates should insist the intellectual property and knowhow of the products they fund is shared in the WHO pool.
The WHO’s attempt to organise a global system where treatments are allocated equitably is also vital. Its efforts should be supported by a framework that places equitable allocation at the heart of all decision-making – including the moment when companies first sign funding agreements with governments and health agencies. But if the WHO is to be successful in the face of vaccine nationalism, we must also do absolutely everything we can to maximise supply. Aside from insisting on the sharing of knowledge and intellectual property, rich countries should be urgently financing the rapid expansion of safe manufacturing capacity in developing countries.
This extraordinary moment calls for a better approach than our current regime of monopoly rights. Only then will we be able to discover and produce, as quickly as possible, a people’s vaccine.
Winnie Byanyima is executive director of UNAids and UN undersecretary general.